Bed Sores in Hospital
Introduction to bed sores
Bed sores in hospitals are an often overlooked condition that affects between 4% and 10% of people in hospitals in the UK. Yearly, around 186,617 develop one or more bed sores during a stay in Hospital.
Bed sores are not typically life-threatening, but they can significantly negatively impact the quality of your life and well-being while you are hospitalised. So what’s the solution? Is there such a thing as being completely free from developing a bed sore?
This article will discuss how a patient can develop and prevent bed sores in a hospital. I hope you find the information here helpful. Please leave feedback in the comments below, and feel free to share examples of your bed sore stories with us.
What are bed sores?
A bed sore is a skin ulcer caused by someone lying in the same position for long periods.
Bed sores can take many forms, ranging from small red spots on the skin to deep ulcers with exposed bone or tissue beneath them. Some people have only one or two localized areas where they experience discomfort; others may have multiple lesions spread across their bodies.
Bed sores are a common problem for people in hospitals or other long-term care facilities. They’re also a risk factor for residents of nursing homes and assisted living facilities and people at home with family members who may be unable to help them as much as they need.
Common names for bed sores
There are many different terms commonly used for Decubitus Ulcers in the UK.
Decubitus ulcers
Decubitis Ulcer is the medical term for a bed sore. ‘Decubitus‘ refers to the position someone lies while in bed. ‘Ulcers’ are sores that are slow to heal, can take many forms and occur on the skin or inside the body.
Bed sores
Bed sore is the most common term for Decubitus Ulcers in the UK. However, it’s important to note that bed sores can also be caused by prolonged pressure from sitting in a chair or wheelchair.
Pressure sores
Pressure sore is another common term for Decubitus Ulcers in the UK.
Bedsores
You will sometimes see bed sores written as bedsores with no space.
Pressure ulcers
Again, a pressure ulcer is a common term in the UK, but typically not as common as ‘bed sore’ or ‘pressure sore’.
Pressure injuries
Probably the least commonly used term for a Decubitus Ulcer in the UK.
The four stages of bed sore development
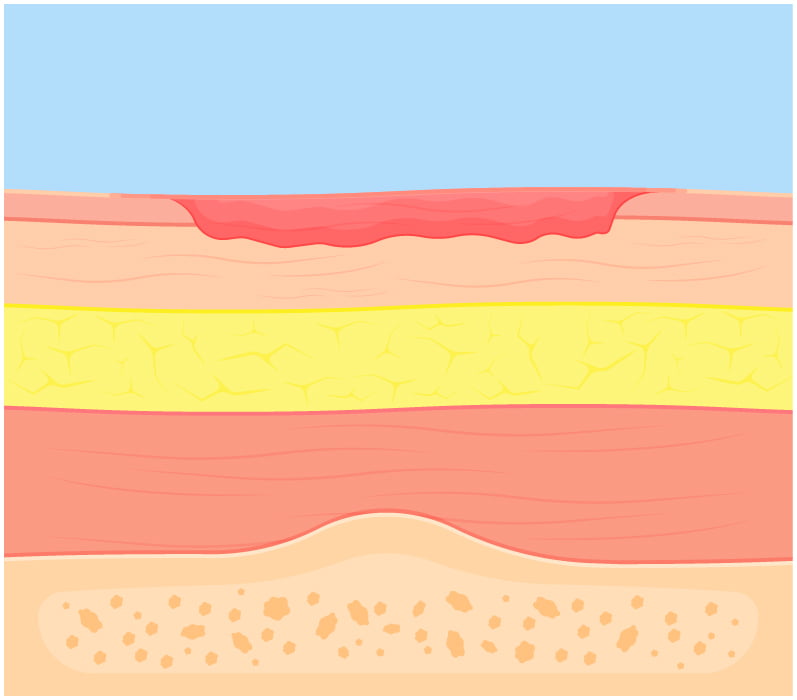
Stage One
Skin reddened and may be warm to the touch and feel firmer or softer than the surrounding skin.
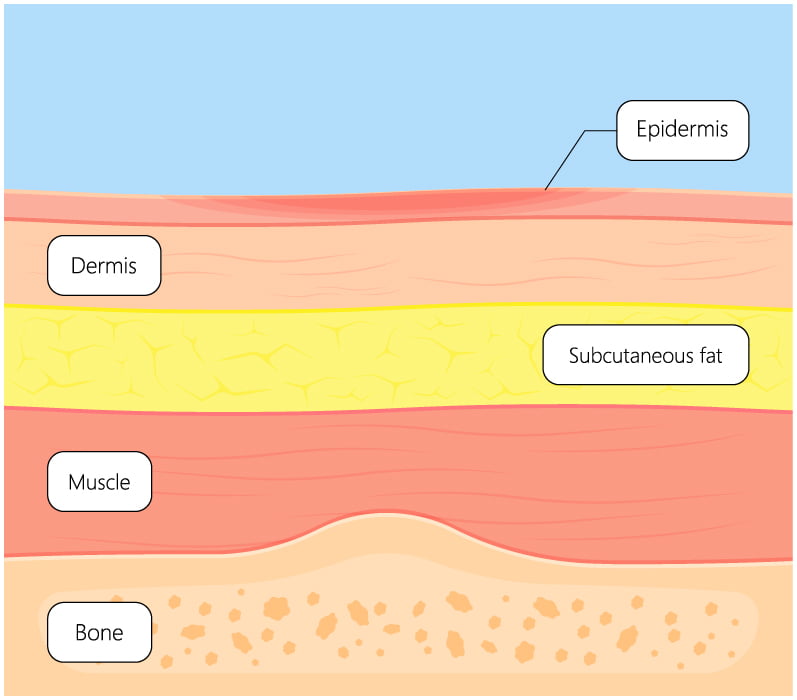
Stage Two
Skin breaks open and exposes the epidermis or dermis. The lesion will be superficial and often resemble an abrasion or popped blister.
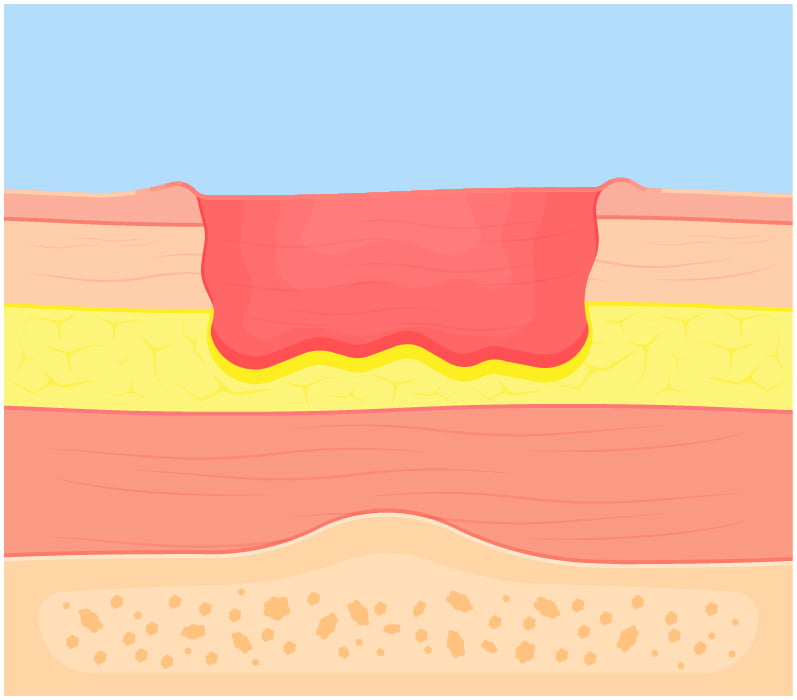
Stage Three
The lesion extends into the dermis and spreads to the subcutaneous layer. At this stage, the lesion will form a small crater. Fat may begin to show in the open sore.
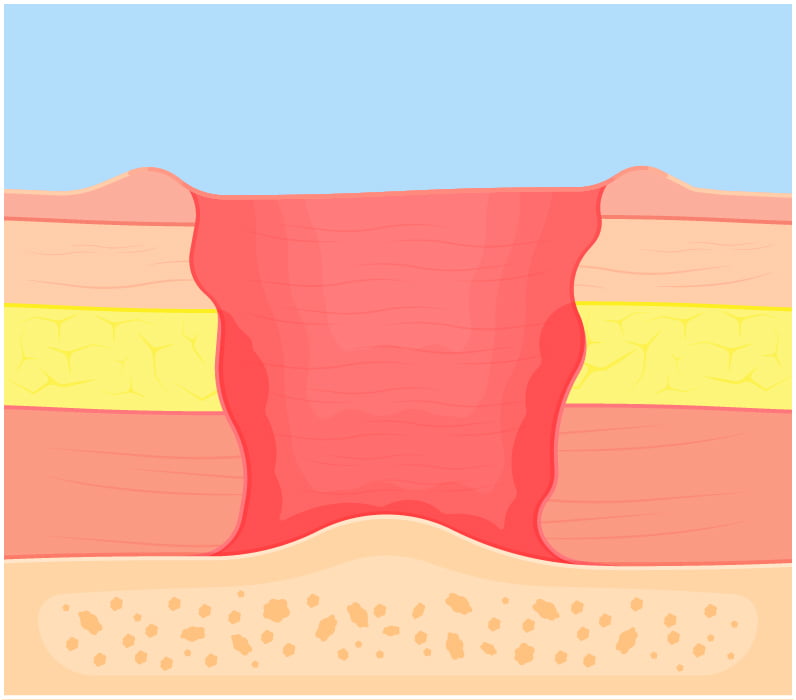
Stage Four
The subcutaneous layer and underlying fascia are breached, exposing muscle and bone.
How might you develop bed sores in Hospital?
To get a bed sore, you need to be in a position where your weight is on one part of your body (usually your bottom or hips) for an extended period. Bed sores can happen if you stay in one position for too long, like if you’re bedridden or sitting up all day with no breaks.
Some people have a higher risk of developing pressure ulcers. Age, diet, hydration and certain medical conditions can cause a greater risk of developing a bed sore. We’ll talk more about specific risk factors later.
Hospitals and Care Homes have a duty of care for their patients and can be liable if their patients develop pressure ulcers while in their care. Typically, you can make a legal claim if the pressure ulcer is stage three or higher.
Parts of the body that are most commonly affected
Certain body areas are more likely to develop pressure ulcers, so checking them regularly when sitting or lying down for prolonged periods is essential.
It’s typically a boney area that is most likely to develop a pressure sore, especially if it supports your weight. Here’s a list of the most likely places for sores to develop:
- Buttocks (tailbone)
- Hips
- Heels of feet
- Shoulder blades
- Backs and sides of knees
- Back of the head
How serious are bed sores?
You can die from bed sores if not treated promptly. The most significant risk factor for a pressure ulcer becoming life-threatening is infection. Thankfully, life-threatening complications from pressure ulcers are infrequent.
However, the tissue damage caused by pressure ulcers can be debilitating and cause significant pain.
Pressure ulcers need to be treated promptly and professionally to ensure a healthy recovery and prevent the ulcer from developing further.
Top Tip: Make sure you take photos and keep a diary of the bed sore(s) development if you or a loved one develops a bed sore while under the care of a medical professional. This evidence will be vitally important if you make a legal claim.
Bed sore risk factors
Several factors increase the likelihood of developing a pressure sore. Knowing the risk factors enables you to assess your risk. If you believe you are at risk of developing pressure ulcers while in the hospital, talk with your doctor or health care professional about minimising your risk.
Prolonged pressure
Prolonged pressure is the leading risk factor for developing pressure ulcers. When the skin has pressure applied over a long time, the blood supply gets cut off, allowing pressure sores to form.
Poor nutrition
Poor nutrition can lead to bed sores. Patients who are malnourished and have a poor diet, or patients who have a poor diet because they’re in the hospital, are at risk of developing pressure ulcers.
Bony areas
Bed sores are more likely to develop on bony body areas, such as the heels, ankles, hips, elbows, and shoulders. These areas don’t have much fat to protect them from pressure. We recommend that you use pressure relief cushions for these areas whenever possible.
Elderly patients
Elderly patients are more likely to develop bed sores because their skin is more fragile, and they have less body fat than younger patients (which means they’re more likely to experience pressure). There’s also an increased risk of infection in elderly patients due to weakened immune systems.
Body fat
The less body fat someone has (even if they’re not underweight), the more likely they’ll develop bed sores—that’s because fat cushions against pressure on your skin which helps prevent damage from occurring underneath it.
Fragile skin
Fragile skin is another factor that makes it easier for bed sores to develop. If your skin is thin or damaged from an injury, it will take longer for wounds to heal and may become infected more easily.
Cold skin
Cold skin also increases your risk of developing pressure ulcers because it does not have enough warmth or moisture for healing tissue.
Diabetes
People with diabetes are particularly at risk for developing these painful wounds because of their decreased circulation and increased pain sensitivity. Diabetes can also impair the body’s ability to heal from skin damage, so good aftercare is vital for minimising the risk of infection.
Preventing pressure ulcers
Let’s take a look at some ways that you could avoid bed sores.
Change position
You should change your position every hour or two to prevent pressure sores. This will help keep your skin healthy and moisturized. It also helps with circulation and prevents muscle aches and numbness.
Healthy diet
A healthy diet is another essential part of preventing pressure sores; eating well helps keep your skin healthy and supports your overall health. Eating healthily reduces the likelihood of fatigue or other symptoms that could make staying comfortable difficult (like nausea). Ensure you’re eating plenty of fruits and vegetables and fibre-rich foods.
Make sure your diet includes plenty of vitamin C and omega-3 fatty acids. These nutrients help keep your skin healthy and elastic.
Drink water
Water helps keep your body hydrated and healthy overall, reducing the risk of developing a pressure sore or similar problems associated with immobility, like deep vein thrombosis (DVT). Dehydration can cause blood vessels to become constricted and lead to poor circulation.
You may want to try drinking an electrolyte-balanced beverage like Gatorade or coconut water for the extra mineral and hydration benefits!
Reduce pressure
Ensure you have enough padding under your body, so it doesn’t rest directly on a hard surface. This includes pillows and mattresses with sufficient support for different parts of your body (such as hips/shoulders) while sleeping or sitting upright.
Use proper body positioning to help spread your weight and support your entire body. Ask your doctor or nurse practitioner to show you how to learn more about doing this!
Healthy skin
Wash daily with mild soap and warm water; pat your skin dry gently with a towel instead of rubbing vigorously. Clean skin will reduce the risk of infection and keep your skin hydrated.
It’s essential to ensure you’re getting plenty of vitamin D, as this is one of the essential vitamins for healthy skin. Vitamins C, E and K also play a vital role.
Sleep
It seems a bit counterintuitive when you consider maintaining the same position for long periods can cause pressure ulcers. However, sleep is vital for our body’s ability to heal. Ask your nurse to help you turn at night to reduce your risk of developing sores.
Risk Assessment
If you’re at risk of developing bed sores, your caregiver should provide a risk assessment with actionable steps to reduce your risk of developing a bed sore. The risk assessment should include instructions that hospital staff must follow to reduce the likelihood of you developing a pressure ulcer.
Check in with your caregiver regularly to ensure they’re checking for sores and changing dressings as needed.
If you develop pressure sores while in the hospital and your caregivers did not follow your risk assessment, you may be entitled to compensation. Make sure you keep records of the care you’re being provided and when your bed sores develop.
Who is responsible for preventing pressure ulcers while in Hospital?
Preventing bed sores is a team effort; everyone is responsible. While in a hospital, the primary responsibility lies with your care professionals, usually your nurses and doctors.
However, you are also responsible for following your caregiver’s instructions and providing them with accurate information about your health. If you’re unhappy with the care you receive while in the hospital, contact your local GP and record your concerns.
Treating bed sores
If left untreated, bed sores can become a very serious problem and even, in rare cases, lead to death (caused by the spread of infection). Here are some tips to help you treat mild bed sores – but make sure you also consult your doctor and follow their instructions.
Pressure sores are treated by protecting the skin from further damage and cleaning and dressing the wound. Pressure sores often take a long time to heal, which can be painful.
You should first check the skin for open wounds and pus to treat a pressure sore. If there is pus drainage, you should clean the skin with soap and water and apply antibiotic ointment to prevent infection. If there is any movement around the wound area, you should use a soft gauze bandage or other dressing.
Contact your doctor immediately if the sore is not healing, getting worse, or causing pain. They can prescribe antibiotics and stronger pain medication. Sometimes further professional medical intervention may be necessary, like removing dead tissue.
Making a medical negligence claim for a bed sore
If your bedsore has developed to stage three or greater you might be able to claim compensation for your bed sore injury. If you would like to learn more about the process of making a medical negligence claim, we have an article called how long does a medical negligence claim take, where you can learn more about the ins and outs of medical negligence claims.
We have a team of compassionate medical negligence and bed sore experts ready to help you out if you would like to make a claim. Feel free Get in touch with us if you want a free claim assessment.

